Systemic Denial After Surgery: A Survivor’s Report of Sabotage by UnitedHealthcare
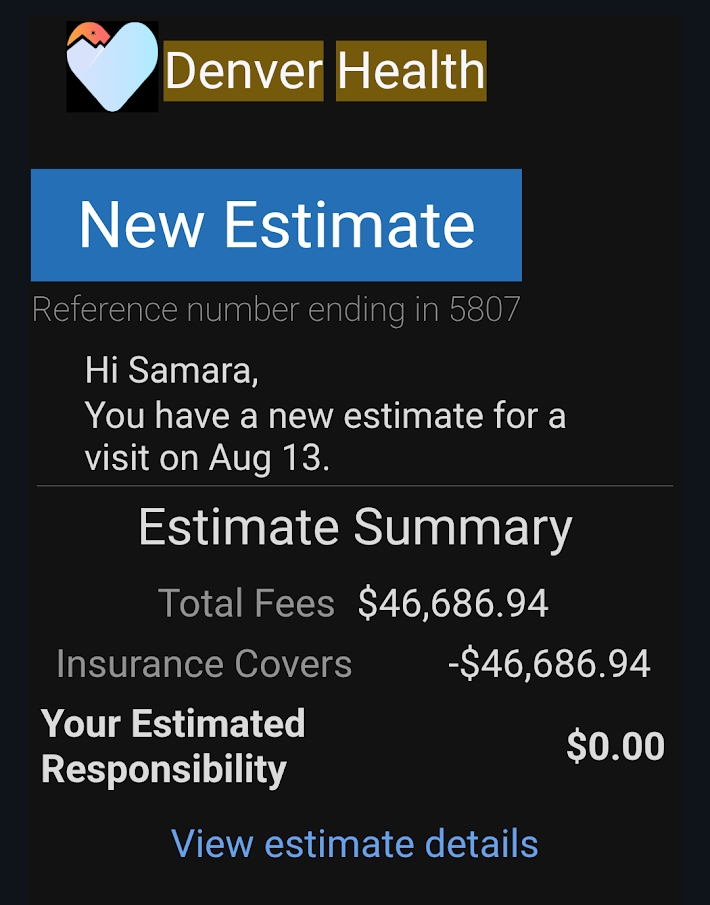
📅 Surgery Date: August 13, 2024
🏥 Facility: Denver Health
💰 Cost of Procedure: $46,686.94
🧾 Covered by Insurance: 100%
🔐 Insurer: UnitedHealthcare / Rocky Mountain Health Plans
🩺 Post-Surgical Hormone Crash: A Manufactured Emergency What should have been a period of rest and healing became a medical and psychological crisis—not because of my surgery, but because of what happened afterward.
After my gender-affirming bottom surgery, I requested a prescription change from oral estradiol to estradiol valerate injections—a safer option due to my history of blood clots around 2016. This was a medically supported choice made during my once-yearly appointment with my long-term OB/GYN (who has treated me since 2008). My provider wrote a brand-new prescription for injectable estrogen specifically to reduce clot risk post-operatively.
But UnitedHealthcare said no.
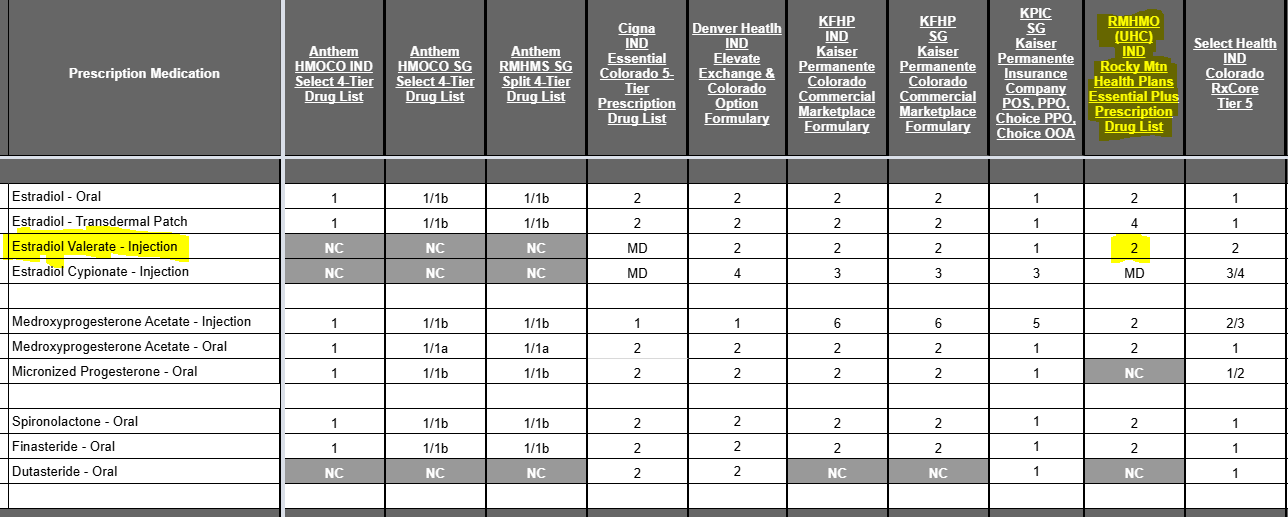
They denied the medication. They claimed it was “non-formulary.” They told my doctor I didn’t need it.
Let me be absolutely clear: this wasn’t about dosage. Estradiol vials have a hard 28-day discard rule after being punctured—something coded directly into the pharmacy packaging (see ⬇️). This was about power and ideology, not medicine.
💊 Hormone Crash: Physical and Psychological Breakdown When United denied my prescription, I was forced to ration old pills—cutting my dose to make them last. The crash was brutal: 😵💫 Extreme dissociation, mental fog
😢 Emotional collapse and intensified depression
🥵 Hot flashes, fatigue, night sweats
😡 Rage, irritability, panic
🧠 Cognitive shutdown—loss of focus, memory, and control
This wasn’t a minor inconvenience. It was a full-body, full-mind, full-spirit collapse—engineered by an insurance company that had no medical justification to interfere.
And I wasn’t the only one.
🧑⚕️ OB/GYN Resistance: Fighting Back Against Discrimination My OB/GYN did everything right. She submitted multiple prior authorizations—at least three. All denied. At one point, we spent over an hour on a joint conference call with UnitedHealthcare, trying to plead with them to follow the law. She pushed. She explained the blood clot history. She explained the discard window. She fought.
United refused.
Eventually, out of desperation, she sent in a script for oral estradiol again. United approved the pills. Not because they were safer. (They aren’t.) But because they could feign “compliance” while still denying what I truly needed.
Finally, on December 12, 2024—three full weeks later—they approved my injectable script.
📦 What Stockpiling Looks Like After Betrayal
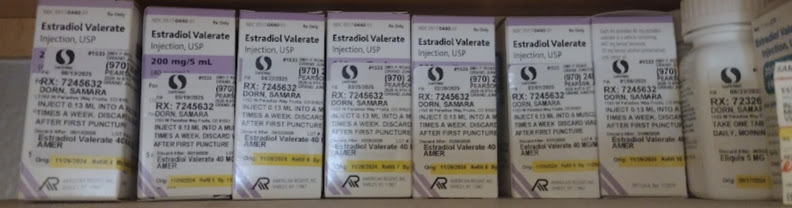 What you see above is seven unopened vials of estradiol valerate. That’s 35mL—because I don’t trust them. Because I don’t feel safe. Because if United takes this away again, the consequences wouldn’t just be clinical. They’d be existential.
What you see above is seven unopened vials of estradiol valerate. That’s 35mL—because I don’t trust them. Because I don’t feel safe. Because if United takes this away again, the consequences wouldn’t just be clinical. They’d be existential.
I am stockpiling my survival. Because I know what it feels like to be cut off. And because I know they’ll try again.
❌ This Was Not a Glitch. It Was a Political Attack. UnitedHealthcare didn’t just violate ethics. They violated the law.
Under C.R.S. § 10-16-104.3(3)(b), Colorado law prohibits health insurance carriers from denying coverage for gender-affirming care when such care is:
“Prescribed or recommended by a licensed health care provider and medically necessary to treat a condition related to the individual’s gender identity.”
The Plaintiff’s injectable estradiol valerate prescription—issued by a long-term OB/GYN provider following gender-affirming surgery—met every requirement under this law. There was no lawful basis for denial.
The Colorado Division of Insurance (DOI) has also issued formal guidance clarifying that:
Formulary exclusions may not be used to deny transition-related care, including hormone therapies.
📍 Legal citation: “Per DOI Bulletin B‑4.126 (2022), insurers may not exclude gender‑affirming hormones from formulary, nor may they deny coverage based solely on route or dosage. United’s denial of injectable estradiol violated both this guidance and state law.”
Insurers must provide equivalent alternatives if a specific formulation (e.g., injectable versus oral) is denied.
Dosage differences alone cannot be a valid basis for denial when a 28-day expiration cycle, not daily usage, determines refill needs.
🔬 Evidence: 28‑Day Limit on Multi‑Dose Injectable Vials Medical and regulatory authorities uniformly affirm that the expiration—or beyond-use date (BUD)—for opened multi-dose injectable vials is 28 days, unless explicitly extended by the manufacturer. This standard governs safety and refill necessity, regardless of dose frequency or remaining volume.
- United States Pharmacopeia (USP) Chapter <797> According to USP <797>, the primary authority for sterile compounding:
“Chapter 797 of United States Pharmacopeia recommends up to 28 days as the beyond‑use date for opened or ‘entered’ (i.e., needle‑punctured) multi‑dose vials of sterile pharmaceutical injection containing antimicrobial preservatives.” — American Regent Estradiol Valerate Prescribing Information, citing USP <797> standards.
- FDA Guidance The U.S. Food and Drug Administration reinforces this rule in its official labeling guidelines:
“The beyond‑use date … for an opened or entered … multiple‑dose container is 28 days, unless otherwise specified by the manufacturer.” — FDA: Labeling Guidelines for Injectable Products (21 CFR § 201.57)
- CDC Injection Safety Protocols The Centers for Disease Control and Prevention (CDC) injection safety guidelines mirror this requirement:
“Multi-dose vials must be dated and discarded within 28 days after first use, unless the manufacturer specifies otherwise.” — CDC Safe Injection Practices Coalition
Want PROOF? CLICK!
📌 Legal Relevance: UnitedHealthcare’s refusal to refill estradiol valerate based on remaining volume ignores these mandatory safety protocols. The refill necessity is governed by expiration timing, not dose consumption. Once punctured, the vial becomes unsafe for use after 28 days—even if hormone remains.
Any denial that fails to acknowledge this standard violates basic medical safety and undermines state and federal gender-affirming care mandates, including Colorado’s statutory protections under C.R.S. § 10-16-104.3(3)(b).
UnitedHealthcare violated each of these principles. They denied coverage for a medically necessary, legally protected treatment—despite a valid prescription, a supportive provider, and a medical rationale rooted in blood clot risk and post-operative care. They forced the Plaintiff to ration medication, suffer physical and emotional harm, and eventually seek an alternate formulation—one that carried greater health risks.
This was not clinical decision-making. This was
Deliberate Sabotage.
And it was illegal.
These denials weren’t just “miscommunications.” They were targeted and systematic.
How do I know?
Because other trans friends in Colorado—different doctors, different prescriptions—had the same thing happen:
❌Denials of testosterone
❌Denials of estrogen
❌Denials of post-op appointments
❌Hours of appeals that led nowhere
❌Psychologically destabilizing delays
And all of this started in the weeks after my surgery.
🏛️ Coordinated Timeline of Political Retaliation Let’s match the timeline:
August 13, 2024: My bottom surgery is performed.
October 16, 2024: Donald Trump declares: “On the first day we will revoke Joe Biden’s cruel policies on transgender treatments… we will stop taxpayer funding for transgender procedures and drugs.”
December 12, 2024: Then-CEO of UnitedHealth Group Andrew Witty states: “We will continue to guard against unnecessary care.”
Those words are not coincidental. They reflect a coordinated political and corporate agenda. To label gender-affirming care as “unnecessary.” To withhold it. To eliminate access by weaponizing bureaucracy.
This wasn’t healthcare.
It was a purge.
It was administrative erasure in action.
⚖️ Intentional, Retaliatory, and Illegal UnitedHealthcare’s actions were not a mistake. They were a calculated breach of trust, law, and bodily autonomy. They used insurance denial as a method of elimination—of denying care, breaking spirits, destabilizing recoveries, and pushing trans people out of the system entirely.
And it worked—for a while.
But now I’m speaking.
This is not an isolated grievance. This is part of a pattern. It is deliberate, documented, and legally indefensible.
United broke the law. They knew what they were doing. And they did it anyway.
✊ You Don’t Get to Erase Me Quietly.
If you’re reading this, then the defendants didn’t settle.
They chose silence.
They chose denial.
They chose the gamble.
But here I am. 📢 Still talking. Still posting. Still surviving. And now, the world gets to see what they did.
#AdministrativeErasure
#HormoneJustice
#SurvivorNotSilenced
#UnitedHealthcare
#RockyMountainHealthPlans